Understanding Shoulder Pain
Things to remember | The shoulder | Causes of shoulder pain | Signs and symptoms of shoulder pain | Diagnosing shoulder pain | Treating shoulder pain | Surgery | Self-management | When to be concerned | The future | Where to get help | How we can help | More to explore | Download PDF
Things to remember
- Shoulder pain is a common problem
- There are many things that can cause shoulder pain
- For most people, it will improve over time with appropriate treatment
Shoulder pain is common in our community. In younger people, pain is more likely to be due to an accident or injury. However as you age natural wear and tear occurs in the shoulder joint and the rotator cuff tendon. This may become persistently painful over time.
The good news is that with appropriate treatment pain will improve so you can get back to doing the things you enjoy.
The shoulder
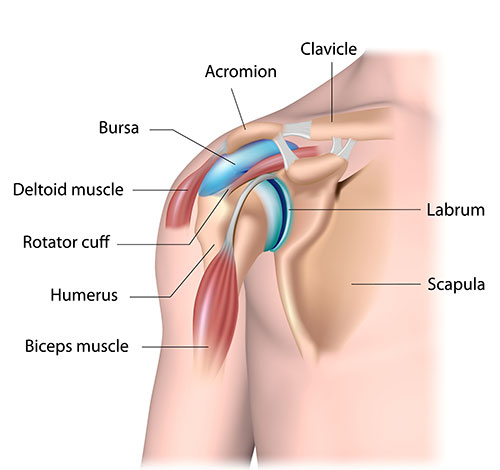
Your shoulder is a complex, highly mobile structure made up of several components. There are two joints:
- glenohumeral joint – where your upper arm bone (the humerus) connects with your shoulder blade (scapula)
- acromioclavicular joint – where the top of your shoulder blade meets your collarbone (clavicle).
Strong connective tissue forms your shoulder capsule. This keeps the head of the humerus in place in the joint socket. The joint capsule is lined with a synovial membrane. It produces synovial fluid which lubricates and nourishes the joint.
Strong tendons, ligaments and muscles also support your shoulder and make it stable.
Causes of shoulder pain
There are many causes of shoulder pain and not all of them are due to problems of the shoulder joints or associated structures.
Osteoarthritis: cartilage is a smooth, cushiony tissue that covers the ends of your bones where they meet in a joint. Healthy cartilage helps your joints move smoothly. Over time cartilage can become worn, or it may become damaged due to injury or an accident, leading to the development of osteoarthritis.
Inflammation of the shoulder capsule
- Synovitis is when your synovial membrane becomes inflamed. It can occur as a result of another condition (e.g. rheumatoid arthritis) or it may happen as a result of an injury. Or the cause may be unknown.
- Frozen shoulder (adhesive capsulitis) is a condition that occurs when your shoulder capsule thickens and becomes inflamed and tight. There may also be less synovial fluid to lubricate the joint. As a result your shoulder becomes difficult to move. Frozen shoulder may occur as a result of another condition (e.g. diabetes), if the shoulder has been immobilised (e.g. due to surgery or injury), or the cause may not be known.
Inflamed bursa: pain associated with an inflamed bursa is also common in the shoulder. A bursa is a small fluid-filled sac that reduces friction between two structures, such as bone, muscle and tendons. In your shoulder the bursa that sits between the rotator cuff tendon and the bony tip of the shoulder (acromion) can become inflamed, most commonly with repetitive movements.
Injuries and sprains
- Ligaments are soft tissues that connect bones to bones. They provide stability to your shoulder by keeping the bones where they’re meant to be. If the ligaments are injured or sprained, they can cause short-term pain. This may be the result of the humerus coming partially out of the joint socket (subluxation) or if the humerus comes completely out (dislocation).
- The flexible tissue that helps keep your shoulder joint in place (the labrum) can become torn. This is called a labral tear. This can occur as a result of an injury (e.g. falling onto your outstretched arm) or repetitive actions (e.g. throwing sports such as cricket).
- A direct blow to your shoulder can result in the acromioclavicular joint being sprained. This type of injury often occurs in people participating in contact sports such as football who take a blow to the shoulder. It can also occur as a result of a fall.
- Rotator cuff: this group of tendons and muscles keep your shoulder stable and positioned correctly for your shoulder and arm to move. Tears to rotator cuff tendons may occur as a result of an injury (e.g. a fall, broken collarbone) or happen over a period of time as you age.
Neck and upper back: problems with the joints and associated nerves of your neck and upper back can also be a source of shoulder pain. The pain from your neck and upper back is often felt at the back of the shoulder joint and/or through to the outside of your upper arm.
Injury to the axillary nerve: this nerve can be injured if you dislocate your shoulder or break your humerus. This can cause weakness when moving your arm outwardly away from the body.
Referred pain: shoulder pain may also be caused by problems affecting your abdomen (e.g. gallstones), heart (e.g. angina, heart attack) and lungs (e.g. pneumonia).
Note: if you feel shoulder pain that is radiating down your arm or you’re experiencing a tight feeling across the chest and shortness of breath, dial 000 immediately.
Symptoms of shoulder pain
There are many causes of shoulder pain, and they all have their own unique set of symptoms.
Depending on the cause of your shoulder pain you may experience:
- pain deep in the shoulder joint, in the back or the front of the shoulder and the upper part of the arm. Sometimes the pain in the shoulder can be described as a ‘catching pain’. The location and type of pain is likely to relate to the structure causing the pain
- reduced movement, and pain when moving your shoulder.
- weakness of the shoulder/upper arm. Depending on the condition, there may be a sensation of the joint slipping out and back in to the joint socket, or the shoulder can become completely dislodged (dislocated)
- sensations of pins and needles (tingling) and burning pain. This is more likely to be associated with nerves from the neck than the shoulder joint itself.
- lack of movement after a shoulder dislocation. This is usually due to pain. Complete rotator cuff tears and injury to the axillary nerve both cause weakness in moving the arm away from the body. These problems require close clinical examination.
Diagnosing shoulder pain
Health practitioners who treat shoulder pain are trained to investigate and identify the exact cause of the condition or injury causing the pain. They will do this by:
- asking about your shoulder pain, including potential causes (e.g. recent injuries, other health conditions), if you have had shoulder pain before, things that make your pain worse, things that make it better
- conducting a thorough physical exam.
From this information they can work out the likelihood of particular structures in the shoulder being involved. Sometimes they will suggest that investigations or tests may be needed.
It’s important to know that many investigations show ‘changes’ to your shoulder that are likely to represent the normal passage of time (even by age 45), not ‘damage’ to your shoulder. An experienced health practitioner can help you to understand the difference.
X-ray
X-rays provide images of your bones and joints. They can show any changes caused by arthritis in the shoulder joint (e.g. bone spurs, narrowed joint space) or fractures. However x-rays don’t show any changes or problems with your soft tissues (e.g. muscles, tendons).
Ultrasound
Ultrasounds are typically used to investigate your rotator cuff tendon for inflammation, tears or rupture. While it can be a helpful tool to use, and can provide clues to identify the source of your pain, a diagnosis can’t be made using the ultrasound alone. If an ultrasound is ordered, then an x-ray should also be arranged. Both tests will provide more complete information about the state of your joints and the tendon.
CT and MRI
Computed tomography (CT) and magnetic resonance imaging (MRI) scans are usually not the first test used to investigate shoulder pain. They may be used when a fracture is suspected or an accident is involved. These scans will help determine the extent of injury and whether further assessment and treatment by a surgeon is needed.
Treating shoulder pain
There are many treatments for shoulder pain:
- physiotherapy – one of the first treatment approaches involves physiotherapy and modifying your activities that make your pain worse. Physiotherapy will aim to fix problems such as stiffness and weakness. It will also include retraining the movements or activities related to your sport, work or everyday activities that were aggravating your shoulder so that wherever possible, you can get back to what you were doing.
- heat and cold packs – may help provide you with temporary relief of pain and stiffness.
- medications – such as paracetamol and low dose anti-inflammatories can be helpful in controlling pain while you work to maintain and restore movement and function. If you have high blood pressure or cardiac or kidney disease, you should talk to your doctor before using these medications. Medications shouldn’t be considered as a long-term solution for your shoulder pain. If your pain persists, you should discuss other treatment options with your doctor.
If your pain persists, your doctor may suggest a corticosteroid injection. While it’s important to understand that all medications have side effects, for most people an injection to help reduce pain while you work to recover is well tolerated. The injection may be repeated once or twice, depending on your circumstances. Keeping a pain diary will help you track how effective it is, and if other forms of treatment are required.
In cases of frozen shoulder, a hydrodilatation may be suggested. This is an injection of fluid (saline and a steroid) into the joint. There is evidence to support this treatment for the relief of symptoms and improved range of motion. Physiotherapy in the days after treatment has been shown to provide further improvements.
Surgery
For most people, shoulder pain will improve over time with appropriate, conservative treatment. However in some cases surgery may be required.
The work that you have already done to try and resolve your shoulder pain (e.g. physiotherapy) is important when facing shoulder surgery. Being informed, and maintaining muscle strength and range of motion leads to better results after surgery. Post-surgery rehabilitation is just as important for good results.
Surgery may be required in the following conditions:
- recurring or frequent dislocations
- acute rotator cuff tears (tears that have recently occurred as the result of an injury)
- chronic rotator cuff tears (tears that occur as a result of wear and tear as you age)
- severe joint damage as a result of osteoarthritis and rheumatoid arthritis.
Surgery for frozen shoulder requires careful consideration as it’s a condition that usually get better naturally over time and can be managed non-surgically. It’s not uncommon for pain and stiffness to persist after surgery for this condition.
Self-management
Most people with shoulder pain will recover from their condition. For many there will need to be a commitment to an exercise-based rehabilitation program. It may also be necessary to make modifications to your lifestyle and work practices that aggravate shoulder pain. Talk with a physiotherapist and occupational therapist for advice.
When to be concerned
It can take some time for shoulder pain to settle, perhaps weeks or months. In general if the shoulder pain has not begun to settle in a week or two then it would be worthwhile seeing an experienced doctor or health practitioner. Worsening pain over time should also be assessed by a doctor.
If you find that stronger opioid medication is needed to manage your shoulder pain, discuss this with your doctor. You may need a referral to a specialist and/or further investigations.
Note: It’s important to note that shoulder pain or discomfort around the front of one or both of the shoulders can be a sign of a heart attack. It’s often described as an ache, heaviness or pressure sensation spreading from the chest to the shoulders. This requires immediate medical attention. Call 000 immediately if you are experiencing these symptoms.
The future
Most people with shoulder pain will find the condition will settle over time. Working with your healthcare team and using self-management techniques will lead to the best outcomes. This treatment may require an experienced physiotherapist to guide you through a comprehensive rehabilitation program.
Where to get help
- Your doctor
- Physiotherapist
- Exercise physiologist
- Occupational therapist
- Musculoskeletal Australia
National Arthritis and Back Pain+ Help Line 1800 263 265
How we can help
Call our Help Line and speak to our nurses. Phone 1800 263 265 or email helpline@msk.org.au.
We can help you find out more about:
- shoulder pain and other musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events.
More to explore
- Better Health Channel
- Choosing Wisely Australia
- National Prescribing Service – Medicine Line 1300 633 424
- TAC
- WorkSafe
Download this information sheet (PDF).
The whole or part of this material is copyright to the State of Victoria and the Better Health Channel. Reproduced with permission of the Victorian Minister for Health. Users are permitted to print copies for research, study or educational purposes.
Information has been produced in consultation with and approved by: Musculoskeletal Australia.
Produced in partnership with Alphington Sports Medicine Clinic