DYK for many years it was believed that ancient Egyptian pharaohs Amenhotep (Amenophis) II, Ramses II (“The Great”), and his son Merenptah all had ankylosing spondylitis (AS)? In 2002, scientists examined X-rays of their mummies and found what they believed were radiological signs of AS. Cool story. And, if you have AS, it’s a mic drop moment. 🎤 Boom!
Unfortunately, this has now been debunked 😑 and the mummies show signs of a completely different condition. But let’s not let facts get in the way of a good story 😁. And let’s find out about AS.
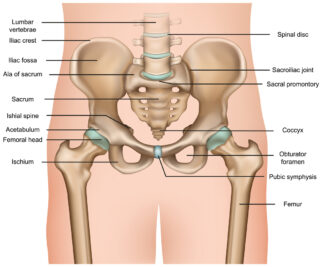
Ankylosing spondylitis is an inflammatory arthritis that causes inflammation in the spine and the joints that connect the lower spine to the pelvis (sacroiliac joints). This inflammation causes back pain, stiffness and reduced mobility in the spine.
The good news is there are effective treatments for AS.
What causes it?
Ankylosing spondylitis is an autoimmune disease. That means it occurs as a result of a faulty immune system.
Instead of identifying foreign bodies (e.g. bacteria, viruses) and attacking them to keep you healthy, your immune system mistakenly targets healthy tissue in and around your joints, causing inflammation and pain.
We don’t know why this happens. Genes are thought to play a role. You’re more likely to get AS if your family has a history of it. Most people with AS have the gene called HLA-B27; however, this gene can also be found in people who don’t have AS.
Since this gene doesn’t automatically lead to the development of AS, scientists believe a complex mix of genes and environmental factors may be involved.
We used to think AS affected more men than women, but recent research suggests men and women are affected relatively equally. AS tends to develop in late teens and early adulthood.
Symptoms
The symptoms vary from person to person. The most common are:
- Pain and stiffness in the back, buttocks or neck, often worse after waking or resting and relieved by exercise and movement.
- Enthesitis, or inflammation and pain where tendons or ligaments connect to bone. Common areas for enthesitis are in the front of the chest where the ribs join the breast bone, the back of the heel (Achilles tendon) or underneath the foot.
- Fatigue or extreme tiredness that doesn’t get better after sleep or rest.
Other symptoms can include:
In AS, due to chronic inflammation, new bone may grow around the joints in the spine. This can lead to permanent stiffness in the back and neck of some people with AS. In severe cases, the bones of the spine can fuse together; however, this can usually be prevented by starting appropriate treatment as early as possible.
Symptoms may change from day to day. At times your symptoms (e.g. pain, fatigue, inflammation) can become more intense. This is a flare. Flares can be unpredictable and seem to come out of nowhere.
Diagnosis
If you have ongoing back pain and stiffness or other symptoms of AS, it’s essential that you see your GP. Getting a diagnosis as soon as possible ensures treatment starts quickly. This will give you the best possible outcomes.
No single test can diagnose AS, so your doctor will use a combination of tests. They may include:
- Your medical history. Your doctor will ask about your symptoms, family history and other health issues.
- A physical examination to assess joint tenderness, flexibility, and stiffness.
- Genetic testing to look for the HLA-B27 gene.
- Blood tests to check for inflammation.
- Scans such as an X-ray and MRI (magnetic resonance imaging) to look for joint inflammation and damage.
Your GP will refer you to a rheumatologist if they think you have AS. Rheumatologists are doctors who specialise in diagnosing and treating problems with joints, muscles, bones and the immune system.
Treatment
Ankylosing spondylitis is treated using a range of different treatments, including medicines, regular exercise and self-care.
Medicines
The two main types of medicines used to treat AS and help manage its symptoms are NSAIDs and targeted therapies:
Non-steroidal anti-inflammatory drugs (NSAIDs) are nearly always used as the first medicine to treat the pain, inflammation and stiffness of AS unless there’s a reason you can’t take them. Research shows that NSAIDs are very effective in managing symptoms of AS. Some people may need to take them regularly, while others will only take them as needed. This will depend on your symptoms and how you respond to the NSAID.
Your rheumatologist will discuss how often you should take NSAIDs and their long-term benefits and risks. There are many different types and brands; some are over-the-counter, while others are only available on prescription.
Targeted therapies are medicines that ‘target’ specific proteins in the immune system that produce inflammation. They include biological disease-modifying anti-rheumatic drugs (biologics), biosimilars and targeted synthetic disease-modifying anti-rheumatic drugs. These targeted treatments have dramatically improved the quality of life for people with AS who need more than NSAIDs to manage their condition.
Your rheumatologist will talk with you about using these medicines if you need more than NSAIDs to manage your condition or if you can’t take NSAIDs.
Exercise
This is the most important thing you can do to help manage your AS. Exercise can improve symptoms, including stiffness, pain, fatigue, breathing capacity and posture. It helps increase your flexibility and range of movement, so it’s easier to do many everyday tasks.
As soon as possible after receiving your diagnosis, you should ideally begin a personalised exercise program developed by a physio or exercise physiologist (EP) and aim to do some exercise every day. Being active is also essential for your overall health and wellbeing. It helps keep your muscles, bones and joints strong so that you can keep moving. It reduces your risk of developing other conditions such as heart disease, osteoporosis, diabetes and some forms of cancer. It boosts your mood, benefits your mental health, helps with weight control and improves sleep.
Self-care
As well as taking your medicines as prescribed and exercising regularly, there are other things you can do.
Learn about your condition. Understanding AS allows you to make informed decisions about your healthcare and actively manage it.
Manage your weight. Being overweight or obese increases inflammation throughout your body. This inflammation affects not only your joints but also blood vessels and insulin levels. This can increase your risk of chronic health conditions such as heart disease and diabetes. Losing weight is an important thing you can do to reduce your risk of these conditions and reduce your AS symptoms. Being overweight or obese also limits the effectiveness of some medicines used to treat AS. Losing weight can be challenging, so if you need to lose weight or advice on healthy eating, talk with your doctor or dietitian.
Learn ways to manage your pain. Pain is the most common symptom of AS, so it’s crucial to learn ways to manage it effectively. Read our A-Z guide for managing pain for more information.
Work closely with your healthcare team. The best way to live well with AS is by working closely with the people in your healthcare team (e.g. GP, rheumatologist, physio). Keep them informed about how you’re doing and if you’ve experienced any changes in your symptoms or tried new medicines, complementary therapies, supplements or other treatments.
Use aids and equipment. Supports such as long-handled shoehorns, reachers and canes can reduce joint strain and make life easier, especially if your condition has reduced your flexibility and mobility. An occupational therapist can advise you on aids, equipment and home modifications.
Sleep well. Not getting enough quality sleep can worsen your symptoms; however, getting a good night’s sleep when you have chronic pain can be difficult. If you’re having problems sleeping, talk with your doctor about how to deal with this.
Manage stress. Stress can also aggravate your symptoms, so learning to deal with stress is extremely helpful. Things you can do to manage stress include planning your day and setting priorities, using relaxation techniques such as going for a walk, getting a massage or listening to music, and, where possible, avoiding people and situations that cause you stress.
Practise mindfulness. Regularly practising mindfulness meditation can improve your mood, relieve stress, improve sleep, improve mental health and reduce pain.
Eat a healthy, balanced diet. While there’s no specific diet for AS, it’s important to have a healthy, balanced diet to maintain general health and prevent weight gain and other health problems, such as diabetes and heart disease.
Quit smoking. Smoking cigarettes harms your general health, negatively affects your bone health, and increases inflammation.
Seek support from others. You might find it helpful to contact the Ankylosing Spondylitis Australia or the Ankylosing Spondylitis Group of Victoria and speak to others who have AS and know what you’re going through.
Complications
Some people with AS develop an eye problem called iritis or uveitis, which causes a painful red eye with blurred vision and sensitivity to light.
If you develop eye symptoms, you’ll need to quickly get your eye checked and treated by an ophthalmologist. Treatment is usually with prescription eye drops, which reduce the chance of permanent eye damage.
Understanding this risk and knowing what signs to be alert for can reduce the risk of eye damage. Ask your GP or rheumatologist what you should do if you develop any eye symptoms.
One last thing
If you think ankylosing spondylitis sounds like a dinosaur, you’re not far wrong. There was a dinosaur called an ankylosaurus. So, what you’ve lost in ancient pharaohs, you’ve gained with a very impressive dinosaur 🐉 😉.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- About the disease
Spondylitis Association of America - Ankylosing Spondylitis
National Institute of Arthritis and Musculoskeletal and Skin Diseases - Ankylosing spondylitis
painHEALTH - Ankylosing spondylitis
Versus Arthritis - Back yourself: Taking control of AS
abbvie - National Axial Spondyloarthritis Society
- Patient education: Axial spondyloarthritis, including ankylosing spondylitis (Beyond the Basics)
UpToDate