Our child has seen so many specialists and now they have been told to go to a kid’s physio. Are you thinking how will a physio help? Or how will this be any different to any other appointments we have? What do I tell my child they will be doing with them?
I am Nicole Pates, a Titled Paediatric Physiotherapist and director of Western Kids Health, a paediatric clinic in Perth Western Australia. I have been a Paediatric physio for over 13 years and these are the things I would like you to know about seeing a paediatric physio.
Children and teenagers, as we all know, are different from adults. Not just physically, but in all of their systems. Their brain is growing and their understanding of their body and how it works is constantly changing. Add into that school, friends and puberty and well, it can be a lot. Let alone managing chronic pain and fatigue on top of this. This is why it is important to work together with a physiotherapist who is experienced in working with kids and teens, who understands growth and development. You can search for a Titled or Specialist Paediatric Physiotherapist, who has undertaken extra study or experience in paediatrics, on the Australian Physio website https://choose.physio/find-a-physio
For families of children with persistent pain and / or fatigue, finding the right help can be tricky. You can find a practitioner experienced in working in paediatric pain on the Australian Pain Society website https://www.apsoc.org.au/Home/wcontent2/60
Once you have chosen a physiotherapist you will be *hopefully* be on your way to an appointment. You may be required to fill out some questionnaires or forms, prior to your initial appointment, depending on your reason for visiting the physiotherapist.
Typically, an initial appointment for children with chronic musculoskeletal / rheumatological conditions will be an hour or potentially more. For some families at Western Kids Health, we might sit down for 2 hours with not just physio but also OT and psychology. I encourage you to contact your chosen clinic to find out more about the first appointment. It is important to dress in clothes that are comfortable to move in and take a water bottle if needed.
Your physiotherapist may ask lots of questions in the first appointment. Not just about your child’s condition, symptoms, history, current team and limitations but also about their strengths, likes and future goals. Your physio will then watch how your child moves and plays, particularly the things they are having trouble with.
We love watching kids move and figuring out the different reasons as to why they might be having trouble or moving differently.
Being able to identify the activities that trigger your child’s symptoms, understanding their experience and watching how your child moves will enable your physio to work with you to formulate a plan. This plan should be collaborative and based around your child’s goals such as getting back to school, sport or hobbies. Having pain or fatigue can be so annoying and make moving and doing things difficult. But with chronic conditions, waiting for the pain or fatigue to go away before you get back into things can be an endless waiting game. Your physio will help you get back into doing things in a way that is meaningful, fun and supported.
Your physio may also provide education around:
- Symptoms such as pain and fatigue and potential triggers / aggravators
- Strategies on how to bring awareness to and strategies to minimise triggers and aggravators
- Why your child may be experiencing pain.
- How best support your child and their pain journey through supportive language in a progressive mindset
Your physio will also work hard to understand where your child’s physical function is at present and work out a plan to build on their activity level, strength, balance, movement control and most importantly, function over time. Your physio will support your child (and you!) with a plan for flare ups or set backs.
Other team members who your physio may recommend supporting you are
- An Occupational Therapist, who assists your child to minimise the impact symptoms may have on sleep, school and relationships
- A Dietician to understand your child’s nutrition needs whilst they are growing and create plans to support and meet these needs
- A Psychologist to build coping skills and resilience and manage mental health symptoms such as low mood, stress or anxiety. This is important as often these symptoms are contributing to or exacerbating your child’s ability to engage in the physical rehab.
At Western Kids Health we run specialised groups in conjunction with the Arthritis & Osteoporosis Association of WA, including group hydrotherapy and strength and conditioning classes.
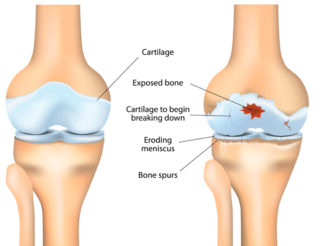
Hydrotherapy and physical conditioning for children with conditions like Juvenile Idiopathic Arthritis is safe and effective. Building strength through range is essential to keep your joints healthy. Your physio will work with you to help your child understand their body’s reactions and sensations as they try new activities. This will help your child build their capacity and understanding of body awareness. Your physio will help explore what movements and types of exercise work best for your child’s body, and most importantly making it fun!
You should see improvements over time with the right support and if you aren’t seeing those improvements, or your child isn’t reaching their goals, please discuss this with your therapy team.
Contact our free national Help Line
If you have questions about managing your pain, your musculoskeletal condition, treatment options, mental health issues, or accessing services be sure to call our nurses. They’re available Monday to Thursday between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- MSK Kids
Musculoskeletal Australia supports children and families with juvenile idiopathic arthritis (JIA) and other musculoskeletal conditions. Check out our full range of resources and support services.