If you’ve ever had bursitis, you know how painful it can be. I had the displeasure of experiencing it several years ago when I slipped in the bathroom and fell heavily. Unfortunately, my shoulder took the full brunt of the fall 😫. I honestly thought I’d broken a bone; it was so painful! But after seeing my doctor, it turns out I had bursitis. And so began several weeks of ice packs, rest and gentle exercise. The good news is that my shoulder recovered completely. But I realised that although I’d heard of bursitis, I didn’t know what this common, painful condition was.
So let’s look at bursitis – what it is, what causes it (apart from falls 😉) and what are the treatment options.
What is bursitis?
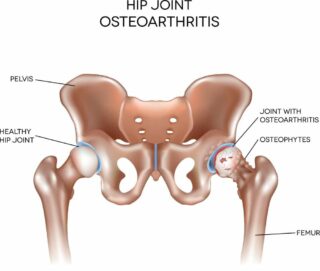
Simply put, bursitis is the inflammation of a bursa. A bursa (plural bursae) is a small fluid-filled sac that cushions your bones and soft tissues (muscles, tendons and skin) in and around your joint.
They reduce friction between moving parts (e.g. between a bone and a tendon), enabling them to move smoothly over each other.
When a bursa becomes irritated or inflamed, it fills up with excess fluid. This causes pain and restricts movement.
What causes bursitis?
Bursitis can develop quickly (acute bursitis) or more slowly (chronic bursitis). Common causes include:
- injury, e.g. having a fall and landing hard on your shoulder or hip
- overusing a joint, especially if the movements are repetitive, e.g. typing, playing tennis
- prolonged pressure, e.g. kneeling for long periods while laying carpet or scrubbing floors
- joint stress, e.g. from being overweight or having an uneven walk (gait)
- other health conditions, e.g. rheumatoid arthritis, gout, diabetes
- infection, e.g. if a joint is injured and bacteria enter the bursa.
What are the symptoms of bursitis?
The signs and symptoms of bursitis include:
- pain, especially when moving the joint
- joint stiffness and swelling
- restricted movement of the joint
- warmth and reddening of the skin in the affected area.
The joints most commonly affected are the shoulder, elbow, hip, knee and heel.
How is it diagnosed?
If you have a painful, swollen joint or you’re finding it difficult to move a joint, it’s important that you discuss your symptoms with your doctor. Getting a diagnosis as soon as possible means that treatment can begin immediately.
To diagnose your condition, your doctor will:
- Take your medical history and ask about your symptoms, recent injuries, the work you do, and other health issues.
- Do a physical examination and look for redness and swelling in and around the joint, and test your joint’s range of movement.
If your doctor thinks your bursa is infected, they may remove a sample of fluid from your bursa. This will be examined under a microscope for signs of infection.
Scans such as x-rays and ultrasounds are usually unnecessary; however, your doctor may send you for a scan to rule out the possibility of another condition.
How is bursitis treated?
Some people can manage the pain, inflammation and stiffness of bursitis with self-care, such as cold packs, rest and gentle exercise. However, other people will require medical treatment to manage.
In this case, your doctor may recommend using over-the-counter non-steroidal anti-inflammatories (NSAIDs). They can be taken as a tablet (orally) or applied directly to the skin (topically) as a cream or gel. In cases of severe pain, your doctor may prescribe stronger anti-inflammatory medicines or inject a corticosteroid into the bursa.
You may also see a physiotherapist or exercise physiologist who can recommend exercises to help your joints move more easily and prevent bursitis from occurring again.
If your bursitis is caused by an infection, your doctor will prescribe antibiotics to treat the infection. In some cases, a needle is inserted into the bursa to remove the infected fluid. This may happen several times until the infection has cleared.
If the bursitis was triggered by a particular form of overuse, it‘s important to avoid that activity or modify how you perform it. An occupational therapist or physiotherapist can help you find solutions to this problem.
What can I do to control my symptoms?
You can do many things to relieve your pain and inflammation.
- Protect and rest the joint to help the bursa recover. Your doctor or physiotherapist will advise you on how to rest the joint and for how long. This could include using cushions or pads when sitting or kneeling for long periods, using a sling or walking stick, modifying your activities etc.
- Ice packs can help soothe red, inflamed joints, and heat packs and rubs can relax tense, painful muscles.
- Maintain a healthy weight to reduce the pressure and stress on weight-bearing joints such as hips and knees.
- Continue to stay active as much as you can while following any instructions provided by your healthcare team to protect your bursa.
- Your doctor, physiotherapist and/or occupational therapist can offer other suggestions and strategies to reduce your risk of developing bursitis again.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- Bursitis
Arthritis Foundation - Bursitis
Johns Hopkins Medicine - Bursitis
MSD Manual Consumer Version - Bursitis
Versus Arthritis - Patient education: Bursitis (Beyond the Basics)
UpToDate