Do you have osteoarthritis in your knees? Does the pain sometimes interfere with your ability to be as quick or mobile as you’d like? If so, you’re not alone – it’s a big club!
Osteoarthritis (OA) is the most common type of arthritis, affecting 1 in 11 Australians. It can develop in any joint but commonly occurs in weight-bearing joints like your knees. And because it’s so common and causes lots of pain and distress, we’re all looking for effective treatments to manage the pain and keep moving.
The good news is there’s strong evidence about the most effective treatments for knee OA, those that aren’t effective, and those that don’t have enough evidence to support their use.
And yet, a recent study has shown an increasing number of people with OA are investigating some less effective treatments such as stem cells, platelet-rich plasma, and Botulinum toxin.
There are likely many reasons for this.
We’ve become much more familiar with searching online for information during the pandemic.
Information about the effectiveness (or not) of treatments isn’t always translated for consumers. And unfortunately, to access much of this information, you need access to journals and databases that are often behind a paywall.
Another problem is that it’s easy for anyone to create a video, blog, or social media post about the latest and greatest treatment without using current evidence. Their reasons for doing so can be many – from sharing personal experiences in the hopes of helping others to purely commercial gain. This info is everywhere online, easily accessible and often looks legitimate.
So you need to weigh any information carefully, be cautious and discuss your options with your doctor.
Here’s a snapshot of what we know works (or doesn’t) for knee OA
Staying active and exercising regularly
You had to know this was coming 😉. Research has repeatedly shown that exercise is key in managing knee OA (and other musculoskeletal conditions). A tailored exercise program developed by a physiotherapist or exercise physiologist can help reduce knee pain and improve knee function. If pain prevents you from exercising, you may find that warm water exercise is a good starting point. Warm water pools offer the comfort of warmth and the buoyancy of the water to ease the load on your joints.
Managing your weight
Being overweight or obese is directly related to the risk of developing knee OA. It’s also likely to speed up how quickly your OA develops or progresses. Evidence shows a relationship between weight loss and relief of symptoms such as pain and stiffness. But weight loss can be a long process for many people. And it’s challenging, especially when pain affects your ability to be as active as you’d like. However, it’s good to know that any weight loss can reduce your pain and increase your ability to exercise. So making small, achievable changes to your eating and exercise habits can bring big results. If you’d like to lose weight to improve your symptoms, your doctor and/or dietitian can assist you in losing weight safely.
Dealing with stress and your emotions
It’s natural to feel stress, anxiety and frustration when living with chronic pain. However, if you’re always fearful or worried about it, it can worsen your pain. That’s because pain isn’t just a physical sensation – it also involves your perceptions, feelings and thoughts.
The worse you think your pain will be, the worse it can feel. It can affect your sleep, and you become less active. These feelings, thoughts and behaviours can become a vicious cycle.
Talking with a family member, close friend, or a health professional about how you’re feeling can get it out in the open so you can start dealing with these feelings and hopefully break this cycle.
Strategies like breathing exercises, cognitive behavioural therapy (CBT), meditation, heat, and gentle activities like tai chi, walking, swimming, and cycling can also help you control your stress and anxiety.
What about medicines?
No medicine can affect the underlying disease process of OA. Still, combined with self-care and lifestyle changes, medicines may provide temporary pain relief and help you stay active.
There are a variety of medicines used in the management of knee OA, and each comes with varying degrees of evidence to support their use. They may be taken by mouth as a tablet or capsule (orally), applied directly to the skin in the form of gels and rubs (topical), or injected into the joint (intra-articular). Discuss the benefits and risks with your doctor if you’re interested in the following medicines.
Non-steroidal anti-inflammatory medicines or NSAIDs (e.g. Nurofen, Celebrex, Voltaren). Depending on the dosage and other ingredients, NSAIDs are available over-the-counter or with a prescription. Oral NSAIDs are the preferred first-line drug treatment for OA and have been shown to reduce pain and symptoms in knee OA.
It’s important to note that NSAIDs are designed to be taken at low doses for short periods. Always talk to your doctor before starting NSAIDs, as they can cause harmful side effects, especially in older people.
Paracetamol (e.g. Panadol, Panamax). Research has shown that paracetamol provides only low-level pain relief and, in some cases, no pain relief compared to a placebo in knee OA. However, some people report that it helps reduce their pain so they can be more active. If you can’t take NSAIDs, they may also be an option. Before using paracetamol, talk with your GP to see if it’s appropriate.
Some medicines aren’t effective
Other medicines have been used for OA in the past that we now know aren’t effective and may have harmful side effects.
Opioids. Opioids are powerful pain-relieving medicines. They’re effective at reducing acute pain (or the pain resulting from an injury or surgery), but evidence shows they have little effect on OA pain. Opioids also have many potentially serious side effects. That’s why they’re not recommended in the management of knee OA.
Capsaicin. Capsaicin is the active ingredient in chilli peppers – it makes them ‘hot’. Capsaicin in creams and lotions has been used to help reduce OA pain, and some people report beneficial effects. However, evidence for its effectiveness in knee OA is low, and it’s generally not recommended. It also has side effects when applied, such as a burning sensation, which can take several uses to wear off.
Glucosamine and chondroitin. Studies have found no benefit from taking glucosamine and/or chondroitin for osteoarthritis.
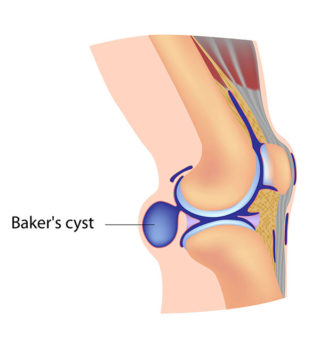
The pointy end of the stick – intra-articular injections
Intra-articular injections are given directly into the knee joint. They include steroids, platelet-rich plasma, stem cells, hyaluronic acid and Botulinum toxin. Let’s look at them a bit more closely.
Corticosteroid injections. If you have persistent knee pain and haven’t had relief from oral medicines or other treatments (e.g. exercise, weight loss), your doctor may suggest a corticosteroid (steroid) injection. However, the duration of pain relief can vary from a few days to a few weeks, and the number of injections you can have is limited due to potential harm. There’s also emerging evidence that long-term use of these injections may cause OA to worsen in the affected joint.
Hyaluronic acid injections. The benefits of hyaluronic acid joint injections (also known as viscosupplementation or hyaluronan injections) are uncertain. Research findings have been inconsistent, and although some people find the treatment helpful, it can be expensive and isn’t generally recommended. The Australian Rheumatology Association states, “emerging evidence indicates that the effect of hyaluronic acid could be smaller than previously reported.”
Platelet-rich plasma (PRP) injections. Platelets are small cell fragments in the blood that help form blood clots to slow or stop bleeding and help wounds heal. PRP is a concentrated version of a person’s platelets injected into the affected joint. An Australian clinical trial led by researchers at the University of Melbourne, University of Sydney and Monash University has found that PRP was no better than a placebo at reducing symptoms in people with knee OA.
Stem cell injections. Despite being commercially available, there’s no evidence for using stem cell injections in treating knee OA. The International Society for Stem Cell Research and the Australian Rheumatology Association do not support using stem cell injections for osteoarthritis.
Botulinum toxin injections. The American College of Rheumatology/Arthritis Foundation Guidelines states that the small number of trials that have looked at the use of botulinum toxin in knee and hip OA ”suggest a lack of efficacy”.(1)
What about surgery?
Surgery may be an option for some people with knee OA when all non-surgical treatment options have failed, and knee pain and reduced function impact their quality of life. In this case, your doctor may refer you to an orthopaedic surgeon to discuss your options.
A total joint replacement of the knee is the most common type of surgery for knee OA. However, having an artificial knee means there will still be some limitations. An artificial knee won’t have the same sideways movement as a natural knee. It won’t bend fully, so getting down and up from kneeling is more likely to be challenging.
Arthroscopy is a surgical technique that involves the insertion of small surgical instruments, including a camera, into the knee. This allows the surgeon to examine the inside of the joint and cut, shave and remove material from the inside of the knee joint. “The Australian Government and most orthopaedic surgeons recommend against using arthroscopy for osteoarthritis of the knee. Research shows that doing an arthroscopy for this condition isn’t effective. Arthroscopy should only be used for knee OA if other treatments fail, such as losing weight, exercising and taking pain relievers.” (2)
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- Cutting through the hype on platelet-rich plasma
University of Melbourne - Duong, V., Hunter, D.J. Osteoarthritis research is failing to reach consumers. Nature Reviews Rheumatology (2023). https://doi.org/10.1038/s41584-023-00972-y
- Jang, C.W., et al. Impact of changes in clinical practice guidelines for intra-articular injection treatments for knee osteoarthritis on public interest and social media. Osteoarthritis and Cartilage (2023).
- Knee health
TREK (Translating Research Evidence and Knowledge) - My knee exercise
The University of Melbourne - Osteoarthritis
PainHEALTH - Osteoarthritis of the knee
Versus Arthritis UK - Osteoarthritis of the knee: A decision support tool for patients considering treatment options
Australian Commission on Safety and Quality in Health Care
References
(1) Kolasinski, S.L., et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis & Rheumatology (2020).
(2) Arthroscopy, Healthdirect