Understanding Osteoarthritis
Things to remember | Your joints | Symptoms | Causes | Diagnosis | Treatment | Exercise | Manage your weight | Medication | Self-management | Surgery | Where to get help | How we can help | More to explore | Download PDF | Translated information | Watch the recording of our webinar on knee osteoarthritis
Things to remember
- Osteoarthritis (OA) occurs when the cartilage inside a joint breaks down causing pain and stiffness
- People over 45 are more at risk, but younger people can be affected too
- Exercise is one of the best ways to manage osteoarthritis.
Osteoarthritis is the most common form of arthritis. It’s most likely to develop in people over the age of 45, but it can also occur in younger people.
OA was once thought to be an inevitable part of ageing, a result of a lifetime of ‘wear and tear’ on joints. However it’s now understood that OA is a complex condition, and may occur as a result of many factors. The good news is that many of these factors can be prevented.
Your joints
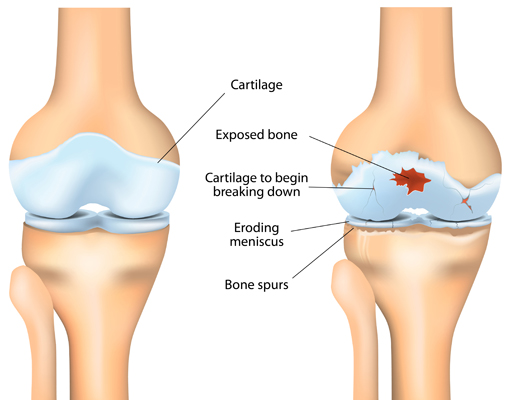
Joints are places where your bones meet. Bones, muscles, ligaments and tendons all work together so that you can bend, twist, stretch and move about.
The ends of your bones are covered in a thin layer of cartilage. It acts like a slippery cushion absorbing shock and helping your joint move smoothly.
The joint is wrapped inside a tough capsule filled with synovial fluid. This fluid lubricates and nourishes the cartilage and other structures in the joint.
With OA, cartilage becomes brittle and breaks down. Some pieces of cartilage may even break away and float around inside the synovial fluid. Because the cartilage no longer has a smooth, even surface, the joint becomes stiff and painful to move.
Eventually the cartilage can break down so much that it no longer cushions the two bones. Your body tries to repair this damage by creating extra bone. These are bone spurs.
Bone spurs don’t always cause symptoms, but they can sometimes cause pain and restrict joint movement.
Symptoms
The symptoms of OA varies from person to person. Some of the more common symptoms include:
- joint stiffness
- joint swelling (inflammation)
- grinding, rubbing or crunching sensation (crepitus)
- joint pain
- muscle weakness.
Causes
There are many things that can increase your chances of developing OA including:
- your age – people over 45 are more at risk
- being overweight or obese
- family history of OA
- significant injury, damage or overuse of a joint.
Diagnosis
If you’re experiencing joint pain, it’s important that you discuss your symptoms with your doctor. Getting a diagnosis as soon as possible means that treatment can start quickly. Early treatment will give you the best possible outcomes.
To diagnose your condition your doctor will:
- take your medical history – this will include finding out about your symptoms, how long you’ve had them, what makes them better or worse
- examine the affected joint/s.
The use of imaging (e.g. x-rays, ultrasound or MRI) and blood tests are not routinely used to diagnose OA. However they may sometimes be needed if there’s uncertainty around your diagnosis.
Treatment
There’s no cure for OA, but it can be managed effectively using exercise, weight loss, medications, and in some cases surgery.
Exercise
Exercise is an important and effective part of any osteoarthritis management plan. Regular exercise can help reduce some of the symptoms (e.g. pain, stiffness) caused by your condition and improve your joint mobility and strength.
Cartilage doesn’t have a blood supply, so it relies on the synovial fluid moving in and out of your joints for nourishment and to remove any waste.
Exercises that involve moving your joints through their range of movement will also help maintain the flexibility that’s often lost as a result of OA.
Strengthening the muscles around your joints is also important. The stronger they are, the more they can support and protect your joints.
Exercise has many other health benefits. It can:
- ease pain and stiffness in your joints and muscles
- improve your balance and posture
- help you sleep better
- improve your mood
- help you maintain a healthy weight, or lose weight when combined with a weight loss diet
- lower stress levels
- reduce your risk of developing other chronic health issues (e.g. diabetes, heart disease).
Talk to your doctor, physiotherapist or exercise physiologist about suitable exercises for you. An exercise program that promotes muscle strength, joint flexibility, improved balance and coordination, as well as general fitness will give you the best results.
Manage your weight
Being overweight or obese increases your risk of developing OA, and the severity of your condition. Additional weight also increases pressure on your joints, especially your weight bearing joints (e.g. hips, knees, feet), which is likely to cause further pain and joint damage.
The amount of overall fat you carry is also important because fat releases molecules that contribute to low but persistent levels of inflammation across your whole body. This in turn increases the level of inflammation in the joints affected by OA.
For these reasons, maintaining a healthy weight is important if you have OA. If you need to lose weight, your doctor or dietitian can advise you on safe weight loss strategies.
Medication
Depending on your symptoms, your doctor may recommend you take medication. They may be over-the-counter or prescription medications.
The most common types used to treat OA include:
- pain relievers (or analgesics) – e.g. paracetamol – for temporary pain relief
- non-steroidal anti-inflammatories (NSAIDs) – e.g. ibuprofen – to control inflammation and provide pain relief
- anti-inflammatory or analgesic creams and gels – may provide some temporary pain relief.
If you’re taking any other medications, supplements or treatments – including any you’ve purchased from a supermarket, health store or complementary therapist – you should discuss these with your doctor.
Steroid joint injections are sometimes recommended for people who still have significant pain after trying exercise, weight loss and/or other medications. However steroid injections can’t be given repeatedly and it’s recommended that you have no more than three to four injections per year in the affected joint.
Self-management
There are many things you can do to manage your OA:
Learn about your condition – knowing as much as possible about your OA means that you can make informed decisions about your healthcare and play an active role in the management of your condition.
See a physio – a physiotherapist can provide you with techniques to improve movement and reduce pain. This can include designing an individual exercise program that’s tailored to your needs, as well as offering advice on ways you can modify your daily activities.
Talk to an OT – an occupational therapist can give advice on pacing yourself and managing fatigue, as well as how to modify daily activities both at home and work to reduce strain and pain on affected joints.
Try relaxation techniques – muscle relaxation, meditation, visualisation and other techniques can help you manage pain and difficult emotions, such as anxiety, and can help you get to sleep.
Seek support – from family, friends, work colleagues and health professionals. A peer support group may be another option.
Grab a gadget – supports such as walking aids, specialised cooking utensils, ergonomic computer equipment and long-handled shoe horns can reduce joint strain. An OT can give you advice on aids and equipment to suit you.
Eat well – while there’s no specific diet for people with OA, it’s important to have a healthy, balanced diet to maintain general health and prevent weight gain and other medical problems, such as diabetes and heart disease.
Stay at work – it’s good for your health and wellbeing. Talk to your doctor or allied health professional about ways to help you stay at work or get back to work
Patella taping, knee braces and orthotics – may be useful if you have OA in your knees or feet. Seek advice from a physiotherapist or podiatrist.
Surgery
In some cases surgery may be necessary if the joint is very painful or there is a risk of losing joint function.
Where to get help
- Your doctor
- Musculoskeletal Australia
National Arthritis and Back Pain+ Help Line 1800 263 265
How we can help
Call our Help Line and speak to our nurses. Phone 1800 263 265 or email helpline@msk.org.au.
We can help you find out more about:
- osteoarthritis and musculoskeletal conditions
- ways to live well with these conditions
- managing your pain
- read our A-Z guide to managing pain
- watch our excellent videos on pain, your brain and how you can retrain your pain system.
- Pain, the brain and your amazing protectometer – Lorimer Moseley
- Treating pain using the brain – David Butler
- upcoming webinars, seminars and other events.
More to explore
- Better Health Channel betterhealth.vic.gov.au
- Australian Physiotherapy Association physiotherapy.asn.au
- Exercise and Sports Science Australia essa.org.au
- Occupational Therapy Australia otaus.com.au
- Dietitians Association of Australia http://daa.asn.au
- Knee osteoarthritis clinical trial Hope4OA www.Hope4OA.com
Download this information sheet (PDF).
Translated information
A simplified version of this information has been translated into the following languages:
- Simplified English (PDF)
- Arabic (PDF)
- Hindi (PDF)
- Punjabi (PDF)
- Simplified Chinese (PDF)
- Spanish (PDF)
- Vietnamese (PDF).
The whole or part of this material is copyright to the State of Victoria and the Better Health Channel. Reproduced with permission of the Victorian Minister for Health. Users are permitted to print copies for research, study or educational purposes.
This information has been produced in consultation with and approved by: Musculoskeletal Australia.