Did you know that there’s a link between certain bacteria and a type of arthritis? It’s strange but true. Find out how a case of food poisoning, or a sexually transmitted infection, can sometimes cause arthritis.
Reactive arthritis (ReA) is a relatively uncommon form of arthritis that occurs as a ‘reaction’ to a bacterial infection in another part of your body.
Usually, when you have an infection, your immune system fights the foreign body (e.g. the bacteria) and then settles down. However, with reactive arthritis, the immune system stays active after the infection has cleared and targets healthy parts of the body, causing pain and inflammation.
Although it’s caused by bacteria, it’s not contagious. However, the bacteria can be passed on to others through sexual activity or contaminated food.
The types of bacteria that cause reactive arthritis are:
- salmonella, shigella, yersinia or campylobacter bacteria – they cause food poisoning and bowel infections
- chlamydia bacteria causes genital infections (though some people may not have any symptoms) and is spread through sexual contact.
Most people who become infected with these bacteria won’t develop reactive arthritis. So the big question is why some people develop arthritis and others don’t 🤔.
Researchers believe that your genes may play a role. You’re more likely to develop reactive arthritis If you have the gene HLA-B27. However, lots of people have this gene and never develop reactive arthritis.
Reactive arthritis can occur at any age, but it tends to affect people aged between 20 and 50.
The good news is that for the majority of people, their condition disappears within 6 months. However, some people experience symptoms for a longer period.
Symptoms
The symptoms of reactive arthritis develop some weeks after the infection and may include:
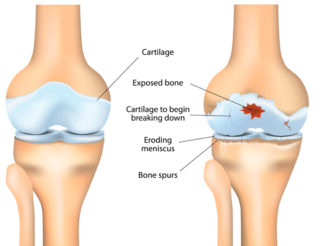
- pain, swelling or stiffness in a joint (arthritis), most commonly the knees, feet and ankles
- pain in the lower back and buttocks
- pain and inflammation of tendons, such as the Achilles tendon at the back of your heel
- pain and redness in your eyes – some people may develop conjunctivitis (inflammation of the outer layer of the eye) or uveitis (inflammation of the middle layer of the eye)
- extreme tiredness, or fatigue
- rash on the palms of your hands or soles of your feet
- mouth ulcers
- diarrhoea.
The good news is most people won’t experience all of these symptoms.
Diagnosing ReA
There’s no specific test for diagnosing reactive arthritis, so your doctor will use a combination of tests to confirm your diagnosis. They may include:
- discussing your medical history – e.g. your current symptoms, as well as any recent illness, infections or other health problems
- a physical examination of your joints, spine, eyes and skin to check for inflammation and other changes (e.g. changes to joint movement, rashes)
- lab tests – e.g. blood, urine or stool (poo) samples may be taken to check for the presence of infection, look for signs of inflammation and to rule out other conditions
- swabs of your throat, penis or vagina to check for signs of infection
- x-rays – may be used to look for signs of arthritis
- arthrocentesis – a sample of fluid is taken from your joint and tested in a lab (this is done to rule out conditions such as gout that may cause similar symptoms).
Treating ReA
Treatment aims to manage the symptoms until you get better and may include:
- Antibiotics to treat the infection. Antibiotics don’t treat the symptoms of reactive arthritis, just the bacterial infection. If you developed reactive arthritis due to a sexually transmitted infection, your sexual partner/s will also need antibiotics.
- Non-steroidal anti-inflammatory drugs (NSAIDs) are the main medicine used to treat reactive arthritis because they quickly reduce joint inflammation and pain. But they do have the risk of side effects, so you’ll be given the lowest effective dose for as short a time as possible to reduce this risk.
- Corticosteroids may be necessary if you have severe joint pain and inflammation. They can be taken as tablets or injected directly into a joint, muscle or other soft tissue.
- Disease-modifying anti-rheumatic drugs (DMARDs) may be given if your condition doesn’t respond well to other treatments. DMARDs suppress your overactive immune system. They help relieve pain and inflammation and reduce or prevent joint damage. It can take several weeks to months before you begin to notice any effect, so you may also need to take other medicines to help control pain and inflammation until then.
- Eye drops to treat conjunctivitis or steroid eye drops to treat uveitis.
- Physiotherapy can help keep affected joints mobile and strengthen the surrounding ligaments, tendons and muscles.
Uveitis requires specialist treatment. If you develop uveitis, your doctor may refer you to an ophthalmologist, a specialist who deals with eye diseases.
Your doctor may also refer you to a rheumatologist, a specialist who treats problems with joints, muscles, bones and the immune system.
Self-care
As well as following the treatment plan your healthcare team has given you, there are many things you can do to manage your reactive arthritis.
Become more informed about your condition. Understanding reactive arthritis allows you to make informed decisions about your healthcare and actively manage it.
Stay physically active. We know that regular physical activity has many health benefits. But it can also help you manage the symptoms of your condition. When you start exercising regularly, you should notice an improvement in your pain levels, the quality of your sleep and an increase in energy levels. However, when your joints are very swollen or painful, avoid strenuous activity or straining the joint. Gentle exercise or movement is best and will help prevent the joint from becoming stiff.
Pace yourself. Pacing is an effective strategy to help you do the things you want to do by finding the right balance between rest and activity (both physical and mental). This will help reduce your risk of flares and fatigue.
Eat a healthy, balanced diet to improve your energy levels, help maintain your weight, and give you a greater sense of wellbeing. And ensure you handle and store your food safely to avoid any contamination.
Learn ways to manage your pain. Pain is a common symptom of reactive arthritis, so it’s important you learn ways to manage it effectively. Read our A-Z guide for managing pain for more information.
Practise good hygiene and safe sex.
Preventing ReA
You can reduce your risk of getting reactive arthritis by avoiding sexually transmitted infections and food-borne bacteria. So:
- Wear a condom during sex with new partners.
- Wash your hands regularly or use hand sanitiser if you don’t have access to water and soap (we’re experts at this now!) 😉
- Make sure your food is prepared and stored correctly.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- Food safety in the kitchen
Nutrition Australia - Patient education: Reactive arthritis (Beyond the Basics)
UpToDate - Reactive arthritis
American College of Rheumatology - Reactive arthritis
Arthritis Foundation - Reactive arthritis
Versus Arthritis