What do a 10th-century Viking/poet, the subject of a 16th-century painting, and an 18/19th-century composer have in common?
Researchers at one time or another speculated they all had Paget’s disease of bone. That the physical features of Egil Skallagrímsson and the Ugly Duchess, and Beethoven’s deafness resulted from living with untreated Paget’s disease.
Later research has thrown shade on these speculations. And in reality, we may never know if they did or didn’t have Paget’s disease. And remember, one’s a painting! But it’s an interesting bit of trivia to store away in the back of your brain. You never know when it might come in handy. 😉
So what is Paget’s disease?
Paget’s disease of bone is a chronic condition that causes abnormal enlargement and weakening of bones. Any part of the skeleton can be affected, but the most common sites include the skull, spine, pelvis, thigh bone, shin and upper arms. It can affect one bone or many bones.
Paget’s disease tends to affect people over the age of 50. It affects slightly more men than women.
Paget’s disease of bone is named after Sir James Paget, a 19th-century English surgeon and pathologist. Paget was quite the go-getter and was the first to describe many medical conditions, several of which bear his name. However, they shouldn’t be confused with Paget’s disease of bone.
Bones and Paget’s disease
To understand how Paget’s disease affects bones, it’s helpful to know how bones work.
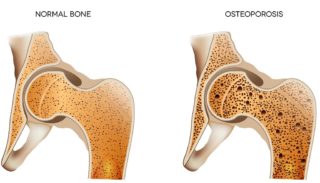
Although we often consider them dry and lifeless, bones are living tissue that are constantly changing throughout life. This is called ‘remodelling’.
Bone cells called osteoblasts build new bone (formation), while other bone cells, osteoclasts, break down and remove old bone (resorption). This process is controlled by hormones such as calcitonin, parathyroid hormone, oestrogen (in women), testosterone (in men), and vitamin D.
In a person with Paget’s disease, the osteoblasts become overactive, producing too much bone tissue. The abnormal growth results in the affected bones becoming deformed (e.g. bowed leg bone), enlarged and weak. The new bone also contains more blood vessels than normal bone.
The reason for this accelerated bone growth is unknown. A combination of genetic and environmental factors (e.g. a virus) is suspected.
Causes, symptoms and diagnosis
As with most musculoskeletal conditions, we don’t know the cause of Paget’s disease. However, some factors increase your risk of developing it. They include:
- Genetics. You’re more likely to develop it if you have a family history of Paget’s disease.
- Ethnicity. It’s more common in people from England, Scotland, central Europe and Greece, and countries settled by European immigrants (e.g. Australia and New Zealand).
- Age. Paget’s disease becomes more common with age, but it’s rare before age 55.
Many people don’t realise they have Paget’s disease because they don’t have any symptoms or only mild symptoms. Symptoms vary but may include:
- bone pain
- enlarged or misshapen bones
- warmth over affected bones due to increased blood supply to the bone
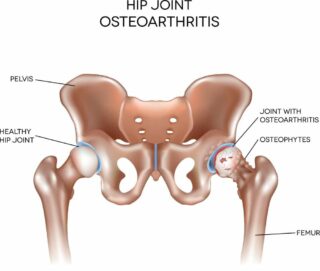
- osteoarthritis.
Paget’s disease is often discovered by accident when x-rays are taken for another reason or a bone is broken. Diagnosis can be confirmed with further x-rays, bone scans or a blood test that checks for an enzyme crucial to bone growth called alkaline phosphatase.
Treatment
There’s no cure for Paget’s disease; however, your symptoms can be effectively managed with medicines and self-care.
Your doctor may refer you to a specialist, such as a rheumatologist or endocrinologist. Rheumatologists are doctors who specialise in diagnosing and treating problems with joints, muscles, bones and the immune system, while endocrinologists specialise in diagnosing and treating problems of the endocrine system.
Medicines.
The types of medicines used for Paget’s disease include:
- Bisphosphonates to slow the progression of Paget’s disease. They help the body control the bone-building process, encouraging more normal bone growth.
- Pain relievers (analgesics) and non-steroidal anti-inflammatory drugs (NSAIDs) to provide temporary pain relief.
Calcium and vitamin D may be recommended as both are essential for good bone health. You can get calcium through your diet and vitamin D through safe exposure to sunlight. If you’re concerned you’re not getting enough calcium and vitamin D, talk with your doctor about whether you need supplements.
Stay active.
Exercise helps maintain bone health and joint mobility and strengthens muscles. However, as bones are weaker and more susceptible to fracture, some exercises may not be suitable for people with Paget’s disease. It’s best to talk with a physiotherapist or exercise physiologist about the most appropriate exercise plan for you.
Enjoy a healthy, well-balanced diet.
This can help you maintain a healthy weight and reduce your risk of other health problems. Make sure you include calcium-rich foods.
Learn new ways to manage pain.
There are many ways to manage pain, and different strategies will work for different situations. Read our A-Z guide for managing pain for more information.
Complications
For most people, Paget’s disease progresses slowly and can be managed effectively. However, in some cases, complications can arise, including:
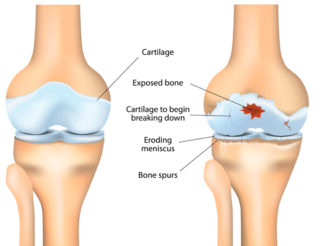
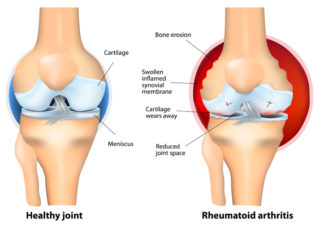
- Osteoarthritis. In joints close to bones affected by Paget’s disease, the cushioning cartilage on the ends of the bones can break down, causing pain and stiffness.
- Broken bones. The new bone growth is fragile and more susceptible to breaking than healthy bone.
- Hearing loss may be caused by pressure on nerves in the ear.
- Numbness or tingling in the spine caused by pinched nerves in the spinal cord.
- Too much calcium in the blood. When several bones have active Paget’s disease, the increase in bone breakdown can lead to an elevated blood calcium level. This is rare, but it can cause symptoms such as fatigue, weakness, abdominal pain, constipation, and loss of appetite.
- Very rarely, Paget’s disease can cause heart failure or bone cancer.
- In severe cases, surgery may be required to relieve pinched nerves or bone fractures or to replace a joint severely affected by arthritis.
Contact our free national Help Line
Call our nurses if you have questions about managing your pain, musculoskeletal condition, treatment options, mental health issues, telehealth, or accessing services. They’re available weekdays between 9am-5pm on 1800 263 265; email (helpline@msk.org.au) or via Messenger.
More to explore
- Paget’s disease of bone
American Academy of Orthopaedic Surgeons - Paget’s disease of bone
American College of Rheumatology - Paget’s disease of bone
Mayo Clinic - Paget’s disease of bone
Versus Arthritis - Patient education: Paget disease of bone (osteitis deformans) (Beyond the Basics)
UpToDate